ACL/Ligament Injury / Reconstruction
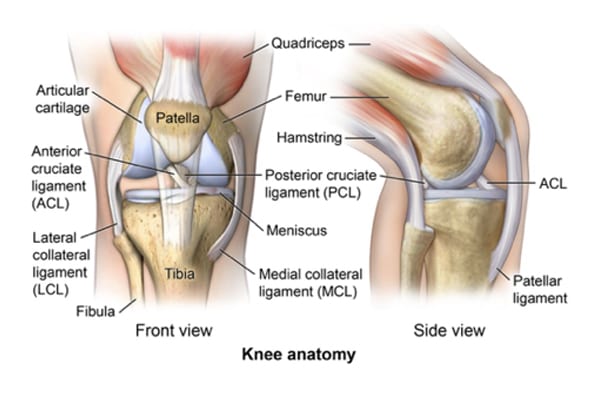
- The anterior cruciate ligament is one of the major stabilizing ligaments in the knee. It is a strong rope like structure located in the center of the knee running from the femur to the tibia. When this ligament tears unfortunately it doesn’t heal and often leads to the feeling of instability in the knee.
- ACL reconstruction is a commonly performed surgical procedure and with recent advances in arthroscopic surgery can now be performed with minimal incisions and low complication rates.
ACL (Anterior Cruciate Ligament)
Anterior cruciate ligament injuries occur most often in the sporting population. A torn anterior cruciate ligament is a common outcome from a major knee injury. The anterior cruciate ligament is the primary stabilizer of the knee joint. Thigh and calf muscles are secondary stabilizers of the knee joint.
If you have torn your anterior cruciate ligament you usually have a sudden twisting movement with your leg fixed on the ground. A snap or pop may be heard and the knee usually swells up within a few hours. The ligament either snaps in half or is pulled from the femoral or tibial surfaces. Once completely torn the ligament cannot repair itself. Partial tears may heal but the ligament is often stretched causing the knee to give way. The anterior cruciate ligament rupture will cause the knee to become unstable in certain movements. This occurs usually when one pivots such as a sudden change in direction. The knee feels like it is going to give way.
At the time of injury, the other ligaments and cartilages in the knee may be damaged. Most commonly the medial collateral ligament may tear and either the medial or lateral meniscus may tear. This may result in locking of the knee joint.
Initial treatment is important to reduce swelling and improve range of motion by appropriate exercises. An x-ray is taken to exclude a fracture and occasionally an MRI scan is arranged to further assess the knee joint. It is quite common to see bone bruising on the MRI scan.
An anterior cruciate ligament reconstruction is recommended in patients whose knees give way on repeated occasions. If you have built up your thigh muscles and your knee does not give way then an anterior cruciate ligament reconstruction may not be necessary. There is a theoretical argument to do an anterior cruciate ligament reconstruction in order to preserve the knee for the future. It has been proven that torn cartilages result in long-term osteoarthritis. It is yet to be proven that a torn anterior cruciate ligament results in osteoarthritis but a torn anterior cruciate ligament with an unstable knee may lead to a torn cartilage and therefore in the end, an arthritic knee. Reconstructing the anterior cruciate ligament may not prevent long-term arthritic changes.
The surgery:
Two methods of anterior cruciate ligament reconstruction are available. The first method uses the central third of the patellar tendon and the second method uses the hamstring tendons from behind the knee. Both methods have advantages and disadvantages and you should discuss with your surgeon his preferred method.
The following steps outline the surgical procedure in anterior cruciate ligament surgery:
- General anaesthetic.
- Hamstring or patellar tendon harvesting and preparation.
- Arthroscopy to clean up the knee joint, trim or repair any torn cartilages and prepare the femoral and tibial bone tunnels.
- The graft is passed through the tunnels and secured either with screws or staples.
- Following anterior cruciate ligament reconstruction, it is important to have a regular physiotherapy exercise program in order to rehabilitate the knee and regain motion. It is most important to regain full extension.
Risks and complications:
General anesthetic risks.
As anybody undergoes general or regional anesthesia (epidural anesthesia) there are always risks associated with it. The risks of course are magnified if you have abnormal general medical conditions, which may have affected the functions of your vital organs such as heart, lungs and kidneys. Therefore, a complete evaluation of those systems has to be performed before you are taken to the Operating theatre.
Specific risks:
- Infection.
- Deep vein thrombosis.
- Numbness just to the side of the incision.
- Stiffness.
- Reflex sympathetic dystrophy.
- Rupture of the graft.
- Damage to vessels and nerves.
- Ongoing instability and pain.


