Shoulder Replacement Surgery for End Stage Arthritis
What is degenerative joint disease of the shoulder?
Degenerative joint disease (DJD) is a pathology of the shoulder in which the articular cartilage between the glenoid cavity of the shoulder and the humeral head at the glenohumeral joint wears down over time causing joint space narrowing, osteophytes, and osteoarthritic pain. Severe physical joint damage can occur if left untreated for an extended period of time.

How does it occur?
DJD of the shoulder’s glenohumeral joint occurs from repetitive, forceful movements of the shoulder and acute trauma. Without treatment, damage to the articular cartilage only worsens over time. As the cartilage wears down, eventually you will have bone on bone contact.
What are the symptoms?
Common symptoms of DJD of the shoulder include persistent pain, instability, trouble lifting, reaching, and the inability to go about your daily activities. These daily activities can involve your work duties, cleaning or working around the house, and playing with pets or loved ones. Eventually you may lose the ability to move your shoulder.
How is it diagnosed?
A detailed history and physical exam will be conducted in the orthopedic clinic. X-rays and an MRI will provide us with a better idea of your underlying shoulder pathology and the extent of any damage present.

How is it treated?
Conservative, non-surgical methods of shoulder pain relief such as rest, non-steroidal anti-inflammatory drugs (NSAIDs), and steroid injections at the shoulder in the clinic may temporarily help, but with end stage degenerative joint disease shoulder arthroplasty (shoulder replacement) may be considered.
Indications for joint replacement surgery are pain you can’t stand it, inability to take care of yourself and perform day to day activities, and inability to do the things you love to do.
In some cases when muscle strength and range of motion is still strong, arthroscopic surgical debridement will be effective to relieve pain and increase function. In these cases, a more conservative minimally invasive surgical approach may be used to avoid a more invasive joint replacement surgery.
Total shoulder replacement replaces the glenohumeral joint in the native anatomical position. The ball of the humerus is restored with a prosthetic metal ball implant, and the glenoid (cup) is replaced with a prosthetic plastic cup that accepts the new metal ball. This method allows your rotator cuff muscles and tendons to control your shoulder movement. If the rotator cuff is extensively damaged a reverse shoulder replacement may be recommended.
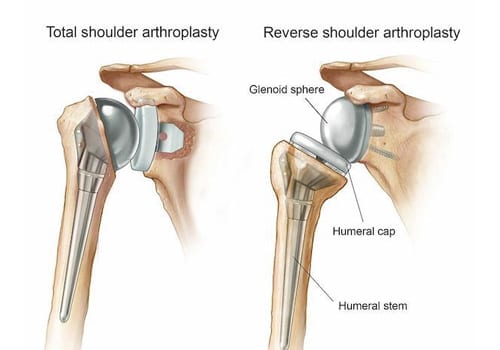
Reverse shoulder replacement is considered a better surgical treatment option for your advanced degenerative joint disease when you have large rotator cuff tears or major rotator cuff arthropathy. When the rotator cuff tendons and muscles do not work properly, a reverse shoulder replacement allows the deltoid muscles to move and power the shoulder. During a reverse shoulder replacement, the top of the humerus is fitted with a metal implant and a plastic cup while the previous glenoid is replaced with a metal ball prosthesis. This reverses the native anatomy but is the optimal treatment for you if indicated to give you the best functioning.
What is the recovery time?
Most patients go home the same day with a few staying overnight. You will come out of surgery with a sling that typically can be removed in 24 hours. Based on the condition of your shoulder, your surgeon will direct you in the appropriate activity levels for your recovery. Once you remove your sling, you begin doing simple range of motion exercises at home. You will do home exercises three times a day and will be evaluated at your 2-week follow-up appointment for progress. We will advance you to Phase II exercises at this time and may advise you to start outpatient physical therapy after your 2-week appointment. Most of our patients are able to have a full recovery with the simple home exercise program Dr. Bramlett has developed. Light duty activity can be started right away, with progression to more strenuous activity in a few weeks with a full recovery in about 3 months. This can vary based on the severity and chronicity of the condition.
We are here to help. If you believe you are suffering from one of these conditions, we would love to deliver a diagnosis, get you treated and get you moving again.


