Separation of the Ball and Socket of Your Shoulder
What is a dislocated shoulder?
The shoulder is made up of three joints: acromioclavicular (AC) joint, sternoclavicular (SC) joint, and glenohumeral (GH) joint. A dislocation of the acromioclavicular joint is a separated shoulder, a dislocation of the sternoclavicular joint is the interruption of the clavicle and the breast bone, and a dislocation of the glenohumeral joint is when the top part of the humerus (humeral head) is misaligned from the glenoid surface.
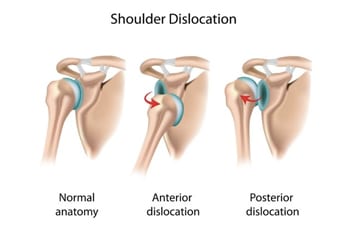
Shoulders can be dislocated anteriorly or posteriorly. The direction of dislocation depends on the type of injury. The shoulder can be partially dislocated called a subluxation or totally dislocated.
How does it occur?
Shoulder dislocations commonly occur from falls, direct blows to the shoulder, trauma, seizures, or electric shock. Other shoulder pathology such as a glenoid labral tear can put you at risk for a shoulder dislocation even when performing normal activities as the labrum acts as an internal stabilizer.
What are the symptoms?
The most common symptoms of a shoulder dislocation are pain, swelling, bruising, limited movement, grinding sensation, and deformity or asymmetry of the shoulders that is obvious to you or others. Patients with shoulder dislocations usually feel the need to support the affected arm.

How is it diagnosed?
Most dislocations are diagnosed through a physical examination and X-rays
How is it treated?
The initial treatment for a shoulder dislocation is reduction, which is putting the humeral head back in the glenoid socket. This is usually done in the emergency department under sedation. The patient is then put in a sling and follows up in the orthopedic surgery office. Further surgery may be needed if instability continues or any other ligament injury is diagnosed with a CT scan or MRI.
Shoulder dislocations in young people are more serious than in the over 60 group as they are more prone to have traumatic ligament injuries. Overall, most dislocated shoulders can be treated conservatively with progressive physical therapy support.

What is the recovery time?
Recovery varies based on the extent of the condition of the dislocation and the healing process of the patient. Our patients usually wear a sling until follow up in the orthopedic surgery office with gradual transition into physical therapy. Most patients can be back to light-duty work in 1 week with possible return to full-duty work in 2 months.
We are here to help. If you believe you are suffering from one of these conditions, we would love to deliver a diagnosis, get you treated and get you moving again.


