Hip Replacement Surgery
The goal of hip replacement surgery is to relieve pain and to improve function and stability. Hip surgery is commonly performed for reasons such as osteoarthritis, rheumatoid arthritis, avascular necrosis, trauma or problems from birth.
Degeneration of the hip joint can affect people of all ages. In the young, it often begins due to trauma in an automobile/motorcycle accident, football injury, falling off a horse or bicycle, or medication which causes the bone to lose its blood supply (avascular necrosis). It can be caused by gradual eroding diseases such as rheumatoid arthritis or lupus. The most common cause is simply normal wear and tear of the cartilage over a lifetime of use, and it is called osteoarthritis. In order to be considered for a total hip replacement there will be three major reasons to have surgery. These are the severe pain you cannot stand it, inability to participate in activities you wish to do, and fear of falling.
Artificial hips last anywhere from one year to twenty years with an average life of 15 years. Since some bone is lost with each replacement, it is better to be in your 50’s or 60’s if possible before having your first hip replacement; however, we know that this is not always possible. To insure the longest life possible for your artificial joint, it is best to maintain a normal weight and avoid abusive activities, such as running for exercise.
A regular x-ray of your hip will give us a realistic picture of what has happened to your bone. The x-ray, the history you give, and a physical examination of your hip will help your surgeon diagnose your condition. Even with all the sophisticated diagnostic tools available today, an x-ray is all that is needed majority of the time.
In the early stages of hip disease (degenerative joint disease), a program of exercise, such as a recumbent bike, swimming, weight control, and non-steroidal anti-inflammatory drugs (NSAIDs), can help decrease the need for surgical treatment. For people under the age of 50, conservative treatment is important to try to delay the need for the hip replacement until they are older. When conservative measures are no longer helpful and one meets certain criteria including weight and strength capacity, a total hip replacement can be the answer.
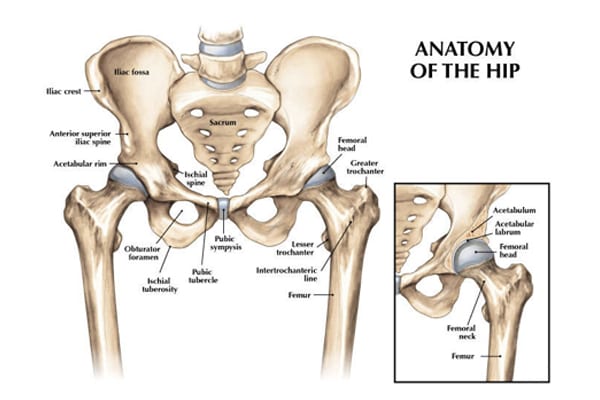
When a hip replacement is decided upon, a combination of metal and plastic are implanted to create a new joint that will glide painlessly with a greater range of motion than one has had in years. Many different prostheses exist, and specific details about you dictate the type selected. The metals used are extremely strong metals designed specifically for use in orthopedic surgery. Polymethyl-methacrylate (PMMA, commonly called “bone cement”) may also be used to hold the acetabular and femoral components in place. Dr. Bramlett’s patients commonly receive a high-strength alloy hip through a minimally-invasive technique avoiding internal muscle disruption.
For total hip replacement surgery, an incision is made down the lateral part of the hip, 4-6 six inches long, depending on how thin you are. The femur and hip socket/acetabulum are exposed. The smallest amount of bone possible is removed and replaced with the metal and plastic components chosen for you. When the joint has been tested for maximum flexion and extension and your surgeon is satisfied with the stability of the knee (the hip does not dislocate easily), it is closed (with a drain sometimes in place). A dressing is applied, and you are taken into the recovery room. The surgery and transfer off the operating room table takes approximately 30 minutes.
Complete recovery should be obtained within 2-6 months; yet, this is dependent on one’s health history. Physical and emotional preparedness prior to surgery are essential. The average is 3 months. Most patients progressively return to their normal activities within 5 weeks, even though, healing will continue for weeks after that. Within a year you will forget you have an artificial hip. You may still have some stiffness with weather changes or increased activity, but your daily life will be much improved. Better quality of life is the main goal for this surgery. Eliminate pain and gain confidence in range of motion and function.
As with any type of surgical procedure, there are certain risks associated with hip surgery. These problems include dislocations, infection, swelling, blood clots, leg length discrepancy, nerve palsy, vascular injury, fractures, and pulmonary embolus. Rare complications do sometimes occur. Extensive measures are taken to prevent each of the above. You will be instructed in measures that will help to decrease the likelihood of problems and aid in a safe healing process. Your cooperation is vital in preventing many of the above complications.
You will be instructed to exercise to build up your stamina and strength and to diet or maintain a normal weight. This can be accomplished by swimming daily and/or riding a recumbent bicycle every other day for 30 minutes. Your cooperation is vital in your recovery process.
Total hip replacements are excellent procedures when chosen and performed correctly on appropriate patients. Your surgeon can provide you with information regarding the specific procedure and implant selected for you.
We hope that you find this information helpful. If any of the material mentioned in this booklet is confusing or hard to understand, you may contact the office with any questions.
Thank you for taking the time to read this material. We understand that this manual contains a great deal of information. We also know that the best results come from the most informed patients and those motivated to see themselves in their best condition as quickly as possible.
Information needed Before surgery
- Total hip patients sometimes need to have a medical check-up before surgery with an internist or primary care physician. If you have any type of heart, kidney, or lung conditions, or you have had heart surgery, you will need to obtain a medical clearance letter from your physician. This is suggested in order to prevent any acute changes in your condition from occurring and will serve to insure a safer, less complicated hospital stay.
- If your medications change from the time of your office visit until your surgery, please notify the office. It is always wise to keep a complete list of your medications and allergies with you, especially when coming to the hospital. If you have not gone to Pre-Admission Testing (PAT) you will need to bring all medicine bottles to the hospital on the day of your surgery.
- If you are taking aspirin or an arthritis medication such as Naprosyn, Aleve, Advil, Ibuprofen Lodine, Voltaren, Feldene, Motrin, Relafen, or Daypro, you should stop taking it 5 days prior to your surgery date. You may continue Tylenol. If you are on Coumadin, Xarelto, Lovenox, Eliquis, Pletal, Pradaxa or any prescribed medication which thins your blood you should check with your primary care physician or cardiologist to see how soon you can get off your blood thinner before surgery
- If you smoke/vape or use any type of nicotine product, we want you to stop at least two weeks before surgery. Smoking increases the risk of respiratory problems and other complications that impede the healing process. The cessation of smoking will enhance the overall improvement of your health and give your body the maximum opportunity to recover without complications.
- DO NOT EAT, DRINK, (NOT EVEN WATER OR ICE), SMOKE, CHEW GUM, OR EAT HARD CANDY after midnight the night before surgery. If you take any stomach, thyroid, or blood pressure medication in the mornings, you should take these with a sip of water the morning of your surgery. Pre-Admission Testing (PAT) will also go over which medications you should take the morning of your surgery.
- Work on the exercise program two times a day every day until surgery. Try to ride a recumbent-chair bicycle every other day for approximately 30 minutes.
- Arrange for family or friends to help you after being discharged from the hospital for the first week. A daily visitor or family member to assist with meals and a shower will make the transition easier. Please start preparing to return to a safe, familiar home environment. If you do not have any help, please let us know. Home Health Care or a rehab facility can be arranged at the hospital by a nurse case manager on the day of your surgery. Please check with your insurance to see if it covers these services.
- You will need to start showering with Hibiclens, Phisoderm, or Dial soap three days before your surgery. This will help guard against infection.
- Our office will call you 1-7 days before your surgery to discuss your arrival time for surgery. Please call us if you have not heard from us within 24 hours prior to your surgery. Surgery times cannot be determined sooner due to surgery schedule changes and emergencies. Please disregard any e-mail you receive stating a time to arrive at the hospital for your surgery.
- Each hospital day is carefully planned, yet changes are not always predictable. Please be patient if your surgery or discharge is delayed.
- You will prepare to come to the hospital the day of your surgery. Upon arrival at the hospital you will check in at the admitting desk in the main lobby of the hospital.
- The average hospital stay for knee surgery is 1 or 2 nights.
- As with all medical information in this manual, please be sure to consult your surgeon’s office if questions exist. All details are beneficial to the overall clinical outcome.
What you SHOULD bring to the hospital:
- If you have your own crutches or walker, please bring them, and be sure to put your name on them. The hospital therapists will make needed adjustments. Otherwise the hospital will provide you with a walker or crutches.
- Bring loose fitting clothes. Your leg will be swollen following surgery. The day after surgery you will start dressing in these clothes instead of a hospital gown. We suggest a loose pair of shorts, a very loose pair of slacks or jogging pants, shirts, and comfortable walking shoes.
- Insurance cards unless you provided the hospital with this information at Pre-Admission Testing.
- Medications you are currently taking. Please bring the bottles if you did not go to Pre-Admission Testing.
- Bring a copy of the results of tests such as EKGs, Echocardiograms, stress tests, and clearance letters from your internists and/or specialist. This is in case we don’t receive these in our office via fax.
- Personal items, such as deodorant/toothbrush/razor.
- Living Will, if you have one.
What you SHOULD NOT bring to the hospital:
- Jewelry
- Unnecessary personal valuables
What you will need at home:
- Walker or crutches and a cane (a walker can be given to you at the hospital).
- Large zip-lock bags for ice or ice packs. You may make your own ice mixture by mixing 1 cup of rubbing alcohol and 3 cups of water into a zip lock bag and placing the bag in the freezer. It will be slushy and colder than a normal ice bag.
- Rubbing alcohol for cleaning the incision, along with tape and gauze pads for a dressing.
- Polysporin to apply to your incision IF you have staples.
- Someone to assist you with a shower and meals for a week once you return home
- Tylenol for pain, headaches, or post-operative fever, which is a normal reaction of the body after surgery.
- A safe environment for walking, without loose rugs or cords, etc. Arrange your bedroom so
you can get in and out of bed easily.
- A firm bed that is easily accessible for rest. Chairs with high and firm seats with armrests.
- DO NOT sit in couches or recliners. Patients tend to sit in recliners or couches and reach for objects, which could put the operative leg in the wrong position causing it to dislocate your new hip.
Antibiotics Information
A joint replacement reacts much like a heart valve replacement to bacteria circulation within the blood stream.
It is required that you have an antibiotic before you have any dental/oral procedures for life.
You cannot have any dental work until 3 months after your surgery.
We can call in a prescription or your dentist can do this for you. The antibiotic protocol for implant prophylaxis follows: Amoxicillin 2.0 grams, taken orally one hour before procedure.
For amoxicillin/penicillin-allergic patients:
- Clindamycin Adults, 600 mg given orally one hour before procedure;
- Cephalexin or cefadroxil: Adults, 2.0 grams orally one hour before procedure; or
- Azithromycin or clarithromycin: Adults 500 mg orally one hour before procedure.
General Order of Events Following Surgery of the Knee:
Operative Day: After surgery you will arrive in your room with a dressing covering your incision. You may rest in bed, then stand at the bedside and/or sit in a chair. Make sure you have a nurse or physical therapist help you until you are safe getting up and down on your own. Once alert, we want you up and out of bed. You will be weight-bearing as tolerated with a walker; you will begin walking with the assistance of a physical therapist or nurse. Start doing your post-operative exercises, such as pumping your ankles to help with circulation. Also, press your knees down flat on the bed, locking your quads for extension. It is also time to do the frog abduction exercises. You can move any way that is comfortable for you. Initially you need to ask for help when turning to your side and getting out of bed. When turning from your back to your side be sure to use a pillow between your knees. You will be given a spirometer to use after surgery to help you breathe deeply; use it hourly while awake. You may start using a regular toilet the day of surgery. This will help to keep your lungs clear and prevent lung infections. Our patients get out of bed 3-6 hours post-operatively. After the first 6 hours bedpans and urinals should not be used. Plan on this as it starts the recovery process.
Post-op Day 1: You need to eat all your meals sitting in a chair. Use the bed only for rest or sleep. The nursing staff and physical therapist will check to see if you are doing your exercises correctly. Initially, the physical therapist or nurse will help you get up and walk with you until you are independent. The nursing staff will also be assisting you in transfers from bed to chair if needed. These activities are important to your progress. Your drain will be removed and a smaller Mepilex dressing will be applied to your drain site. The Mepilex dressing on your hip is good for 7 days and will not need to be changed. You may go home after you finish afternoon physical therapy and are medically stable.
Post-op Day 2: You will progress toward independently moving from bed to chair, exercising, and walking with a walker or crutches. You should be out of bed as much as possible You should be getting up every hour during the day for 5-15 minutes. While sitting in the chair, practice lifting your knee and foot off the floor. While in bed, you should be working your legs into the frog position. This is a very safe position and will help you later for putting on your shoes. By consistently practicing this you should obtain a greater range of motion than you have had in years. You will also work on stair climbing. If you didn’t go home post-op day 1, you should be able to be discharged on post-op day 2.
Post-op Day 3: You may take a hot shower the day you go home. Practice all the physical therapy exercises you received from the hospital and our office until you are comfortable performing them. Many hip surgery patients are able to return home on the 1st or 2nd post-op days. Most find home more comfortable once they are independent and medically stable. Hip surgery patients who are planning to go to a rehab facility will be sent post-op day 3.
Post-operative appointment: To insure your safe post-operative progression, your surgeon will ask you to return to the office 12-16 days after your surgery for x-rays and removal of staples, sutures, or tape from Dermabond glue. Your surgeon may ask to see you again at various intervals, for example, 6 weeks, 2 to 4 months, 6 months, and 1 year. For the long term, each patient is evaluated every two years with repeat x-rays and clinical exams.
Information needed AFTER surgery
Once home, with a total hip it is important to get up and move frequently. You need to get up every hour for 5-15 minutes during the day. Hip replacements do well and people thrive on the lack of pain and sudden ability to be active again. Post-operative problems are uncommon, yet it is important to call your surgeon’s office if you have a sudden increase in hip pain, increased swelling which does not decrease in the morning, or drainage from the incision. If you experience chest pain or shortness of breath, you should go to the emergency room immediately.
The following guidelines will apply for the next four weeks or until your surgeon allows changes:
- Use your walker or crutches as instructed until you feel safe and confident enough to go to a cane, crutch, or staff. This could take 1-2 weeks.
- If there are no contraindications, take an 81mg aspirin daily for 30 days after finishing your Xarelto, Eliquis, Plavix, Coumadin, Aspirin 325mg, or Lovenox to decrease the risk of blood clots. If you are on Coumadin, please have your medical doctor do the blood test required to check the levels 2-4 days after discharging from the hospital to regulate the dose. This is very important.
- Use a pillow between your knees to turn in bed for approximately 2 months after surgery.
- Get in and out of bed on the side of the bed nearest to your surgical hip.
- Keep your knees 4 inches apart at all times when moving around for the first 2 months. In any situation, whether sleeping, sitting, getting in and out of the car, be careful to keep your knees apart for the first 2 months. This will enable you to relax and enjoy your hip for a long time.
- When sitting, choose an armchair for the first 2 months and anytime, thereafter if you have an option. It will make getting up and down easier, safer, and extend the overall life of your hip. For the first 2 months, do not sit on couches, low chairs, recliners or in bathtubs.
- An elevated toilet seat is unnecessary due to the method used to insert the hip; however, if your bathroom is a good distance from your bed, it might be helpful to have a bedside toilet to use at night. During the day, the arms of the toilet can be used over your regular toilet to assist you.
- Continue to wear your support stockings (anti-embolism hose) for 4 weeks after surgery. You should not sleep in them. You may request a second pair before you leave the hospital, or you may purchase regular support hose elsewhere.
- You may shower as soon as you go home. We are using a Mepilex or a Silverlon dressing which you will keep on for 7 days. On the 7th day, you will remove the dressing, shower, clean the incision with alcohol to dry the area thoroughly, and apply the Mepilex or Silverlon dressing from the hospital to keep incision clean. Keep this second dressing on for 7 days.
- Surgical stainless-steel staples or Dermabond, a type of glue, are used to close the skin after surgery. The staples or Dermabond tape are removed in the office 12-16 days after surgery. The tape from the glue is a very thin mesh which you can barely see. DO NOT REMOVE THE MESH TAPE. To make the removal of staples easy, apply polysporin to the incision for the two days before the staple removal appointment. If you have Dermabond tape do not use polysporin. You may use Maderma cream, Aloe Vera creams, Vitamin E Cream, or skin lotion on the incision after it has healed completely (approximately 3 weeks). Steri-strips will be applied after removing the staples and left on for 5-10 days. Remember no tub baths until after steri-strips have been removed.
- Ice your hip every hour for 20 minutes after surgery. This will help with the pain and swelling.
Picking Up Objects from the Floor
Begin by practicing standing on the operative leg, squat (bend) slightly on the one leg and hold for a minute. As you get stronger, go lower with the squatting position. Alternate working with both legs. You may start this as early as you want, usually around two weeks. When you feel strong enough to get to the ground safely, begin by holding on to a table, chair, or wall for balance. Kneel down on the knee of your non-operative leg. Once you are stable, bring your other knee down so that you are in a kneeling position. Finally, spread your knees apart. You are in the correct position. To get back up, reverse the process you just followed. Hold onto something for support. It is important to always have someone with you the first few times you practice this technique. You should gain strength before trying this alone. Hold onto a piece of heavy furniture, such as an armchair, with the opposite hand. Stand on the non-operative leg and lift the affected leg (straight) behind you while bending down to pick up the object. You must have good strength in order to do this safely.
Putting on Socks and Shoes
Sit in a chair and put your foot on a stool with knee rolling outward. It is safe to reach and do these activities in this manner. Never put your shoes on by bending at the waist and putting your foot out to the side allowing your knee to bend and roll inward. This can cause dislocation of the hip. Women shaving their legs or applying lotion sometimes use this same improper movement. More problems are experienced following hip surgery by people attempting to do these things than any other activity.
Getting In and Out of a Car
Getting in the car should be done keeping your knees apart at all times. Back into the seat, holding onto the car door and the seat back. Sit down and bring one leg in and then the other. Remember to keep your knees separated, heels turned inward, and knee outward as if you are keeping a ball between your knees. Have the seat pushed as far back as possible and the back of the seat tilted, so you will have more room.


