Recurrent Dislocating Shoudler
What is multi-directional instability of the shoulder?
Multi-Directional Instability (MDI) is a shoulder pathology defined by symptomatic laxity of the glenohumeral joint, meaning shoulder dislocations are common in one or multiple directions (anterior, posterior, and inferior). Patients with MDI have trouble with the top of the humerus (humeral head) staying centered in the glenoid cavity (the cup of the shoulder joint).

How does it occur?
Multiple injuries to the shoulder over time or a severe injury may cause the shoulder capsule, labrum, or rotator cuff to become torn or weak. This places the glenohumeral joint at higher risk for hyper-mobility. Genetic conditions can cause the soft tissue of the shoulder to be flexible enough for recurrent shoulder dislocations to occur, as well. Young females are very susceptible to this condition when playing sports aggressively.
What are the symptoms?
Patients may describe a sensation of the shoulder slipping when performing overhead movements or when carrying heavy objects. Pain and inflammation from other associated shoulder pathology such as rotator cuff tendonitis/tears and impingement syndrome can progress to damage that causes your MDI. A history of multiple shoulder dislocations warrants further investigation into the shoulder pathology causing these dislocations.
How is it diagnosed?
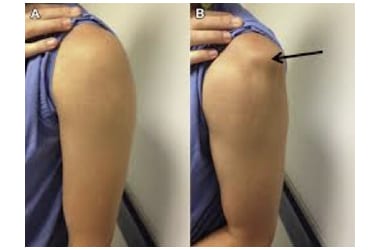
A detailed history and physical exam will be performed in an orthopedic surgery clinic. X-rays and an MRI are important in observing bony structures, as well, as soft tissue structures of the shoulder. Range of motion (ROM) of the shoulder will be assessed, and your shoulder will be felt for any separations or bumps around the bony structures as force is applied in different directions. A positive sulcus sign indicates inferior glenohumeral laxity and is usually present with MDI.
How is it treated?
MDI disease may be treated non-surgically with rest, activity modification, non-steroidal anti-inflammatory drugs (NSAIDs), physical therapy and steroid injections in an orthopedic clinic. The goal is to reduce inflammation that worsens shoulder pathologies causing your MDI. However, surgical intervention may be required to repair the damaged structures allowing the MDI. Minimally invasive arthroscopic surgery or open surgery for repairs are options depending on your shoulder pathology.
Latarjet procedure is commonly utilized in recurrent shoulder dislocations as a result of MDI. This procedure involves the removal and transfer of a section of the coracoid process off the scapula with its muscle attachments to the front of the glenoid cavity. This transferred piece of tissue acts as a bone block and muscle stabilizer so that your humeral head is less likely to dislocate at the front of your shoulder.

MDI is a nuisance condition making a patient frightened every time they perform activities. It can lead to progressive arthritis conditions of the shoulder. If present in middle aged or younger population, it is best to have it repaired.
What is the recovery time?
Since this surgery involves a bone graft, it must be protected during the healing process. You will wear a sling after surgery for the first 2-4 weeks. You may remove it for feeding and grooming/hygiene. Face to waist activity initially which will be advanced to range of motion overhead exercises at four weeks, first with no weight then small hand weights. You will be followed closely through your recovery process, and activity level and rehab exercises will be advanced as deemed appropriate by your doctor. Progressively return to sports activities starting at 12 weeks will be allowed.
We are here to help. If you believe you are suffering from one of these conditions, we would love to deliver a diagnosis, get you treated and get you moving again.


