Plantar Fasciitis
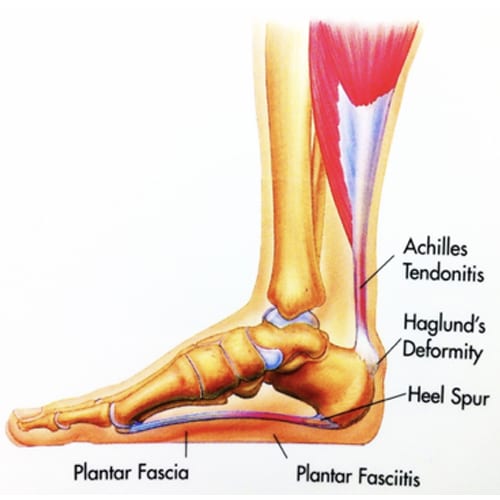
Plantar fasciitis is one of the most common causes of heel pain. It involves pain and inflammation of a thick band of tissue, called the plantar fascia, that runs across the bottom of your foot and connects your heel bone to your toes. The heel pain is worse in the morning when first getting out of bed. Sometimes it will get better the more you walk and stretch your foot. Standing for long periods of time or getting up from a long period of sitting makes the pain worse.
Conservative or Surgical Treatment
Conservative treatment includes changing your shoes, orthotics, stretches, and anti-inflammatories such as Advil or Aleve. Occasional steroid injections can be used for treatment as well. Your pain usually decreases as more walking or stretching is done.
Surgery is often recommended for people who are experiencing constant heel pain which is not helped with anti-inflammatories, exercises, and adequate arch support. Dr. Bramlett does a unique minimally invasive surgical procedure known as an endoscopic plantar fascia release. The goal is to remove scar tissue and the bone spur that is causing constant heel pain.
Incision
There are two ½ inch incisions on the medial aspect of the heel.
Anesthesia
General anesthesia unless contraindicated. If you have general anesthesia, you will be unconscious/asleep throughout the procedure.
Surgery Time
15 to 30 minutes.
Hospital Stay
Approximately five hours. This is an outpatient procedure and rarely do you have to stay overnight.
Average Total Recovery Time
From three to six weeks.
Possible Complications
Infection, nerve and/or circulatory damage, anesthesia risk.
Icing
For the first 2-3 days you can cover your bandaged foot with two sturdy plastic bags and immerse your foot in a bucket or cooler with ice and a little water. You use two bags in case one bag has a hole in it. Do this 3-4 times a day. This is great for swelling and bleeding, and pain. After removing bandages you may ice with ice bags.
Dressing
The first 48 hours you will have a large soft dressing. The dressing can be changed at home or in the office. Please call for an appointment to have the dressing changed in 3 – 5 days and a post op visit 2 weeks post op for suture or staple removal.
Shower
A shower is permitted 48 hours after your surgery. You should rinse your foot with warm water, pat dry, clean incisions with alcohol and re-dress foot with gauze and an ace wrap. Avoid soaking your foot in standing water.
Normal Post-Operative Occurrences
The most common problems are swelling, redness, mild to moderate discomfort, and blood tinged drainage.
Medications
Your prescriptions will consist of pain medication, usually Percocet or Norco and Phenergan or Zofran for nausea if needed. You may resume your anti-inflammatory medicine following surgery. If you do not take any anti-inflammatories, you may take Aleve or Advil with a Tylenol. This helps with swelling and pain control. Pain medication can cause constipation, so increase the bulk in your diet and if needed take a laxative. Over the counter medications like Advil and Aleve are less likely to cause constipation.
Activity/Exercise
Crutches or a walker will be helpful to use until you can walk comfortably. This is usually around 2- 3 days. Elevate your leg on 3-4 pillows above your heart and use ice 20-30 minutes every hour for swelling and pain control.
Driving
You may drive 48 hours after surgery if you have had surgery on your left foot and are off pain medications. Pain medicines may cause drowsiness and inhibit judgment so we recommend you not drive while taking them. If you have had surgery on your right foot you may drive when you can apply your breaks quickly.
Returning to Work
If your job requires minimal walking, you may return to work in 7 to 14 days. If moderate walking is required and light duty cannot be arranged, you should be able to return in 2-3 weeks. If excessive walking is required and light duty cannot be arranged, you should be able to return in 4-8 weeks. Job duties will dictate return to work.
Post-Op Visit: You will need a return appointment 1-2 weeks following surgery for an assessment of your post-operative condition and suture removal. This will need to be on a Monday or Thursday. Please call our office to make an appointment.
Our team has developed this treatment guide in order for you to have a quick reference for your care and recovery. We have made a very simple protocol to enable you an easier recovery. It is my pleasure to be able to diagnose and treat our patients, and we will do whatever is necessary to assist you with your recovery and satisfaction.


