Shoulder Joint Tear (Glenoid Labrum Tear)
Advances in medical technology are enabling doctors to identify and treat injuries that went unnoticed 20 years ago. For example, physicians can now use miniaturized television cameras to see inside a joint. With this tool, they have been able to identify and treat a shoulder injury called a glenoid labrum tear.
Anatomy
The shoulder joint has three bones:
- the shoulder blade (scapula),
- the collarbone (clavicle), and
- the upper arm bone (humerus).
The head of the upper arm bone (humeral head) rests in a shallow socket in the shoulder blade called the glenoid. The head of the upper arm bone is usually much larger than the socket, and a soft fibrous tissue rim called the labrum surrounds the socket to help stabilize the joint. The rim deepens the socket by up to 50% so that the head of the upper arm bone fits better. In addition, it serves as an attachment site for several ligaments.
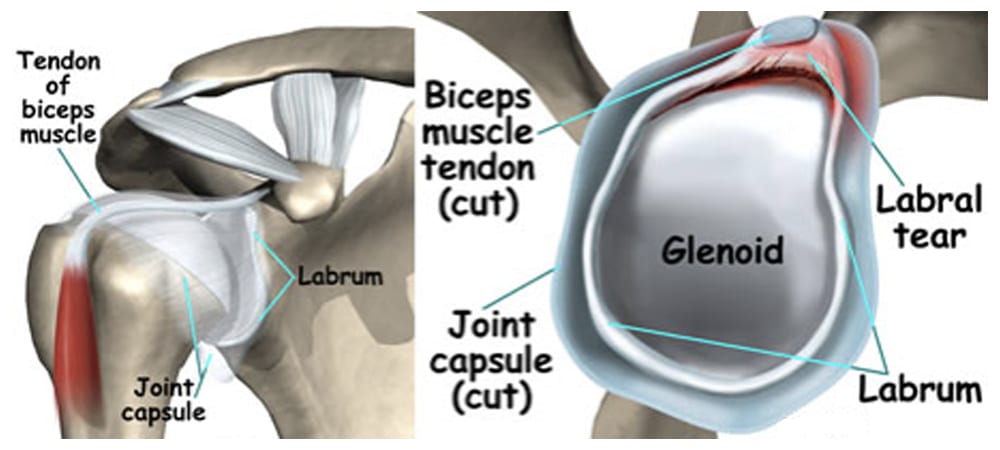
The labrum deepens the socket of the shoulder joint, making it a stronger fit for the head of the humerus.
Cause
Injuries to the tissue rim surrounding the shoulder socket can occur from acute trauma or repetitive shoulder motion. Examples of traumatic injury include:
- Falling on an outstretched arm
- A direct blow to the shoulder
- A sudden pull, such as when trying to lift a heavy object
- A violent overhead reach, such as when trying to stop a fall or slide
Throwing athletes or weightlifters can experience glenoid labrum tears as a result of repetitive shoulder motion.
Symptoms
The symptoms of a tear in the shoulder socket rim are very similar to those of other shoulder injuries.
Symptoms include:
- A sense of instability in the shoulder
- Shoulder dislocations
- Pain, usually with overhead activities
- Catching, locking, popping, or grinding
- Occasional night pain or pain with daily activities
- Decreased range of motion
- Loss of strength
Doctor Examination
If you are experiencing shoulder pain, your doctor will take a history of your injury. You may be able to remember a specific incident or you may note that the pain gradually increased. The doctor will do several physical tests to check range of motion, stability, and pain. In addition, the doctor will request x-rays to see if there are any other reasons for your problems.
Because the rim of the shoulder socket is soft tissue, x-rays will not show damage to it. The doctor may order a computed tomography (CT) scan or magnetic resonance imaging (MRI) scan. In both instances, a contrast medium may be injected to help detect tears. Ultimately, however, the diagnosis will be made with arthroscopic surgery.
- Tears can be located either above (superior) or below (inferior) the middle of the glenoid socket.
- A SLAP lesion (superior labrum, anterior [front] to posterior [back]) is a tear of the rim above the middle of the socket that may also involve the biceps tendon.
- A tear of the rim below the middle of the glenoid socket that also involves the inferior glenohumeral ligament is called a Bankart lesion.
- Tears of the glenoid rim often occur with other shoulder injuries, such as a dislocated shoulder (full or partial dislocation).
Treatment
Until the final diagnosis is made, your physician may prescribe anti-inflammatory medication and rest to relieve symptoms. Rehabilitation exercises to strengthen the rotator cuff muscles may also be recommended.
In many cases, nonsurgical methods are effective in relieving symptoms and healing the injured structures. If these nonsurgical measures are insufficient, your doctor may recommend surgery. Depending upon your injury, your doctor may perform a traditional, open procedure, or an arthroscopic procedure in which small incisions and miniature instruments are used.
During arthroscopic surgery, the doctor will examine the rim and the biceps tendon. If the injury is confined to the rim itself, without involving the tendon, the shoulder is still stable. The surgeon will remove the torn flap and correct any other associated problems.
If the tear extends into the biceps tendon or if the tendon is detached, the biceps tendon may be considered unstable. The surgeon will need to repair or transfer the tendon to a safer location using absorbable tacks, screws, or sutures.
During arthroscopy, your surgeon inserts the arthroscope and small instruments into your shoulder joint.
Tears below the middle of the socket are also associated with shoulder instability. The surgeon will reattach the ligament and tighten the shoulder socket by folding over and “pleating” the tissues.
This procedure may be done arthroscopically or open with a small incision on the front of the shoulder.
Rehabilitation
After surgery, you will need to keep your shoulder in a sling for 3 to 6 weeks, depending on your doctor’s recommendation.
Your doctor will also prescribe gentle, passive, pain-free range-of-motion exercises.
When the sling is removed, you will need to do motion and flexibility exercises and gradually start to strengthen your shoulder.
Athletes can usually begin doing sport-specific exercises 12 weeks after surgery, although it will be 4 to 6 months before the shoulder is fully healed.


