Why a Knee Replacement?
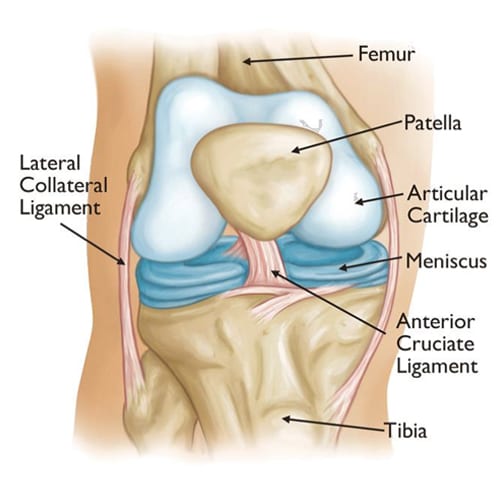
The goal of knee replacement surgery is to relieve pain and to improve function and stability. Knee surgery is commonly performed for reasons such as osteoarthritis, rheumatoid arthritis, avascular necrosis, trauma or problems present at birth.
Degeneration of the knee joint can affect people of all ages. In the young, it often begins due to trauma in an automobile/motorcycle accident, football injury, falling off a horse or bicycle, or medication which causes the bone to lose its blood supply (avascular necrosis). It can be caused by gradual eroding diseases such as rheumatoid arthritis or lupus. The most common cause is simply normal wear and tear of the cartilage over a lifetime of use, and it is called osteoarthritis. In order to consider a total knee replacement there are three indications that it is time to decide to have surgery. These are severe pain you cannot stand, inability to participate in day-to-day activities you wish to do, and instability or a fear of falling.
Total Knee Replacement
Half Knee Replacement
Artificial knees typically last ten to twenty years with an average life of 15 years. Since some bone is removed with each replacement, it is better to be in your 50’s or 60’s if possible before having your first knee replacement; however, we know that this is not always possible. To ensure the longest life possible for your artificial joint, it is best to maintain a normal weight and avoid high impact activities. You can run with a knee replacement after 6 weeks, but it may accelerate wear and tear, requiring revision surgery sooner.
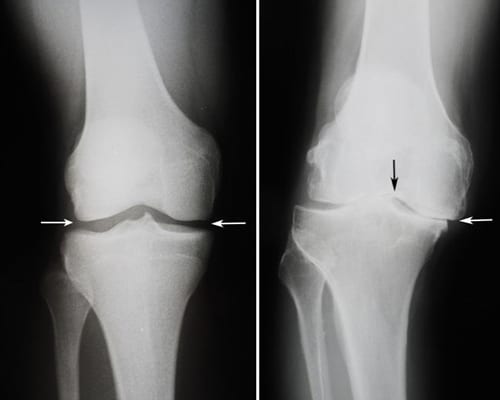
A regular x-ray of your knee will give us a realistic picture of what has happened to your bone. The x-ray, the history you give, and a physical examination of your knee will help your surgeon diagnose your condition. Even with all the sophisticated diagnostic tools available today, an x-ray is all that is needed majority of the time.
In the early stages of knee disease (degenerative joint disease), a program of exercise, such as a recumbent bike, swimming, weight control, and non-steroidal anti-inflammatory drugs (NSAIDs), can help decrease the need for surgical treatment. For people under the age of 50, conservative treatment is important to try to delay the need for the knee replacement until they are older. When conservative measures are no longer helpful and one meets certain criteria including weight and strength capacity, a total knee replacement is the next step.
When a knee replacement is decided upon, a combination of metal and plastic are implanted to create a new joint that will glide painlessly with a greater range of motion than one has had in years. Many different prostheses exist, and specific details about your medical condition dictate the type selected. The metals used are extremely strong metals designed specifically for use in orthopedic surgery. Polymethyl-methacrylate (PMMA, commonly called “bone cement”) may also be used to hold the tibial and femoral components in place. Dr. Bramlett generally does not use a tourniquet if cement is not used, which decreases post op pain and lowers your risk of developing a blood clot.
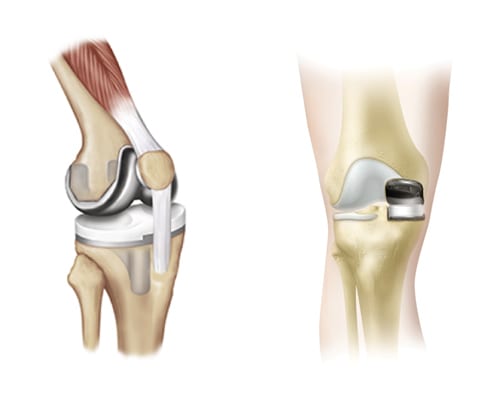
For knee replacement surgery, an incision is made down the middle of the knee, four to eight inches long. The quadricep muscle is left intact, allowing for a quicker recovery. The knee joint is exposed. The smallest amount of bone possible is removed and replaced with the metal and plastic components chosen for you. When the joint has been tested for maximum flexion and extension and your surgeon is satisfied with the stability of the knee, it is closed with a drain in place. A dressing is applied, and you are taken into the recovery room. The surgery itself takes approximately 30 minutes.
We primarily use two different systems to ensure precision cuts giving optimum alignment with minimal bone resection. One is a computer guided electronic gyroscope called iAssist that aligns your knee and hip.
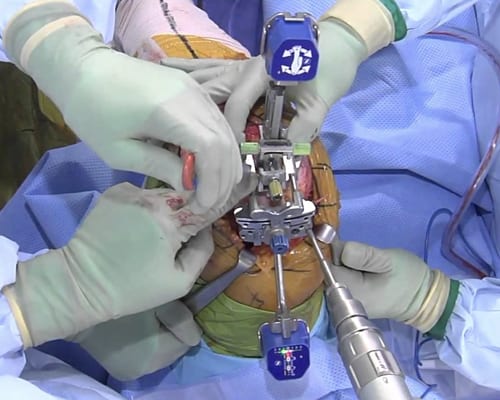
The other system is a robotic assist (ROSA) total knee system. This system assists with bone resection as well as assessing soft tissue balancing to give optimum results.

Both systems are very accurate and reliable. Your surgeon will choose the most appropriate method for your specific clinical condition to give you the best possible results.
Complete recovery should be obtained within 3-6 months depending on your individual health condition. Most patients progressively return to their normal activities within 6 weeks. The healing process will continue for weeks after that. Within a year you will forget you have an artificial knee. You may still have some stiffness with weather changes or increased activity, but your daily life will be much improved. Better quality of life is the main goal for this surgery. Eliminate pain and gain confidence in range of motion and function.
As with any type of surgical procedure, there are certain risks associated with knee surgery. These problems include infection, swelling, blood clots, nerve palsy, vascular injury, fractures, and pulmonary embolus. Rare complications do sometimes occur. Extensive measures are taken to prevent each of the above. You will be instructed in measures that will help to decrease the likelihood of problems and aid in a safe healing process. Your cooperation is vital in preventing many of the above complications.
Total knee replacements are excellent procedures when chosen and performed correctly on appropriate patients. Your surgeon can provide information regarding the specific procedure and implant selected for you.
We hope that you find this information helpful. If you have any questions or need clarification, you may contact us at the office.
Thank you for taking the time to read this material. We understand that this manual contains a great deal of information. We also know that the best results come from the most informed patients and those motivated to see themselves in their best condition as quickly as possible.
Most of the total knee arthroplasties and unicondylar total knee arthroplasties on done as an outpatient where you can go home the same day. We use a Minimally Invasive Surgical Technique developed to decrease complications and ensure a speedy recovery.
Information needed BEFORE surgery:
- Total knee patients sometimes need to have a medical check-up before surgery with an internist or primary care physician. If you have any type of heart, kidney, or lung conditions, or you have had heart surgery, you will need to obtain a medical clearance letter from your physician. This is suggested in order to prevent any acute changes in your condition from occurring and will serve to insure a safer, less complicated hospital stay.
- If your medications change from the time of your office visit until your surgery, please notify the office. It is always wise to keep a complete list of your medications and allergies with you, especially when coming to the hospital. If you have not gone to Pre-Admission Testing (PAT) you will need to bring all medicine bottles to the hospital on the day of your surgery.
- If you are taking aspirin or an arthritis medication such as Naprosyn, Aleve, Advil, Ibuprofen, Lodine, Voltaren, Feldene, Motrin, Relafen, or Daypro, you should stop taking it 5 days prior to your surgery date. You may continue Tylenol. If you are on Coumadin, Xarelto, Lovenox, Eliquis, Pletal, Pradaxa or any prescribed medication which thins your blood you should check with your primary care physician or cardiologist to see how soon you can get off your blood thinner before surgery. You should also stop taking any herbal supplements including fish oil or vitamin E 1 week prior to surgery.
- Tobacco: If you smoke/vape or use any type of nicotine product, you will need to stop at least two weeks before surgery. Smoking increases the risk of respiratory problems and other complications that impede the healing process. Tobacco use is also associated with higher infection rates. The cessation of smoking will enhance the overall improvement of your health and give your body the maximum opportunity to recover without complications.
- DO NOT EAT, DRINK, (NOT EVEN WATER OR ICE), SMOKE/VAPE/TOBACCO, CHEW GUM, OR EAT HARD CANDY after midnight the night before surgery. If you take any stomach, thyroid, or blood pressure medication in the mornings, you should take these with a sip of water the morning of your surgery. Pre-Admission Testing (PAT) will also go over which medications you should take the morning of your surgery. You will need to contact them to schedule.
- Work on the exercise program 2 times a day every day until surgery. Try to ride a recumbent-chair bicycle every other day for approximately 30 minutes. Arrange for family or friends to help you after being discharged from the hospital for the first week. A daily visitor or family member to assist with meals and a shower will make the transition easier. Please start preparing to return to a safe, familiar home environment. If you do not have any help, please let us know. Home Health Care or a rehab facility can be arranged at the hospital by a nurse case manager on the day of your surgery. Please check with your insurance to see if it covers these services. Insurance may only cover inpatient rehab in certain situations.
- You will need to start showering with Hibiclens, Phisoderm, or Dial soap three days before your surgery. This will help guard against infection.
- The hospital or surgery center will call you the day before your surgery to discuss your arrival time for surgery. Please call the hospital OR or surgery center if you have not heard from them the afternoon prior to your surgery. Surgery times cannot be determined sooner due to surgery schedule changes and emergencies. Please disregard any e-mail you receive stating a time to arrive at the hospital for your surgery.
- Each hospital day is carefully planned, yet changes are not always predictable. Please be patient if your surgery or discharge is delayed.
- You will prepare to come to the hospital the day of your surgery. Upon arrival at the hospital, you will check in at the admitting desk in the main lobby of the hospital.
- If your surgery is done at the surgery center you will be discharged a few hours after surgery once you are up and walking and are able to eat, drink, and void. If you have surgery in the hospital you may go home the same day or stay the night. Either way you will be up and walking a few hours after surgery.
- As with all medical information in this manual, please be sure to consult your surgeon’s office if questions exist. All details are beneficial to the overall clinical outcome.
What you SHOULD bring to the hospital:
- If you have your own crutches or walker, please bring them, and be sure to put your name on them. The hospital therapists may make needed adjustments. Otherwise, the hospital will provide you with a walker or crutches if you need them.
- Bring loose fitting clothes. Your leg will have a bulky dressing and can be swollen following surgery. The day after surgery you will start dressing in these clothes instead of a hospital gown. We suggest a loose pair of shorts, a very loose pair of slacks or jogging pants, shirts, and comfortable walking shoes.
- Insurance cards unless you provided the hospital with this information at Pre-Admission Testing.
- Medications you are currently taking. Please bring the bottles if you did not go to Pre-Admission Testing.
- Bring a copy of the results of tests such as COVID test, EKGs, Echocardiograms, stress tests, and clearance letters from your internists and/or specialist. This is in case we do not receive these in our office via fax.
- Personal items, such as deodorant/toothbrush/razor.
- Living Will, if you have one.
What you SHOULD NOT bring to the hospital:
- Jewelry
- Unnecessary personal valuables
What you will need at home:
- Walker/crutches and a cane or staff
- A Game Ready ice machine. This helps tremendously with post op pain and swelling. Dr. Bramlett highly recommends that you rent it for 2 weeks unless your budget doesn’t allow it. The cost is $120 a week and is not covered by insurance. You can return the Game Ready at our clinic when we see you for your follow-up appointment. After you turn in your Game Ready, you may use ice packs. You can make your own ice mixture by mixing 1 cup of rubbing alcohol and 3 cups of water into a zip lock bag and placing the bag in the freezer. It will be slushy and colder than a normal ice bag.
- Rubbing alcohol for cleaning the incision, along with tape and gauze pads for a dressing.
- Polysporin/Neosporin to apply to your incision IF you have staples. Apply the ointment 2 days before coming for your follow-up appointment. Do not use Polysporin on Dermabond glue closures.
- Someone to assist you with a shower and meals for a week once you return home
- Tylenol for pain, headaches, or post-operative fever, which is a normal reaction of the body after surgery.
- A safe environment for walking, without loose rugs or cords, etc. Arrange your bedroom so you can get in and out of bed easily.
Antibiotics Information
A joint replacement reacts much like a heart valve replacement to bacteria circulation within the blood stream.
It is required that you have an antibiotic before you have any dental/oral procedures for life.
This includes routine cleanings and exams.
You cannot have any dental work until 3 months after your surgery.
We can call in a prescription or your dentist can do this for you. The antibiotic protocol for implant prophylaxis follows:
Amoxicillin 2.0 grams, (4x500mg pills) taken orally one hour before procedure.
For amoxicillin/penicillin-allergic patients:
Clindamycin Adults, 600 mg given orally one hour before procedure
Cephalexin or cefadroxil: Adults, 2.0 grams orally one hour before procedure
Azithromycin or clarithromycin: Adults 500 mg orally one hour before procedure.
General Order of Events Following Surgery of the Knee:
Operative Day: After surgery you will have a surgical drain (in some cases), a bulky dressing, and an ice pack on your knee. The ice helps with pain and swelling. Please let your nurse or physical therapist know if you need more ice. You may rest in bed, then stand at the bedside and/or sit in a chair. Once alert, you should begin doing your post-operative exercises by pumping your ankles. Point the toes of your surgical leg to your face, tighten your quads, and press your knee down. You can move any way that is comfortable for you. Early straightening and bending of your knee help you recover faster and decreases pain. Don’t forget you need to ask for help when getting out of bed. You will be given an incentive spirometer to use after surgery to help you breathe deeply; use it hourly while awake. This will help to keep your lungs clear and prevent pneumonia. You may start using a regular toilet the day of surgery. If a surgical drain is used, it will be removed prior to discharge.
If you are ambulating well and your pain is well controlled, you may go home the same day as your surgery. Our prehabilitation program and minimally invasive surgical techniques allow our patients to have a shorter hospital stay and quicker recovery.
Post-op Day 1: You need to eat all your meals sitting in a chair with your legs hanging down allowing gravity to pull them down. Use the bed only for rest or sleep. If you are still in the hospital, the nursing staff and physical therapist will check to see if you are doing your exercises correctly. Initially, the physical therapist or nurse will help you get up and walk with you until you are independent. The nursing staff will also be assisting you in transfers from bed to chair if needed. If you are at home, your support person will help you as needed. Make sure you do not lay in bed all day. These activities are important to your progress. If you are still in the hospital, you may go home after you finish physical therapy and are medically stable. Physical therapy will work with activity level and the hospitalist will clear you medically.
Post-op Day 2: You should be out of bed as much as possible if you went home post-op day 1. You should be getting up every hour during the day for 10 minutes. While sitting in your chair, alternate sitting with your legs on the floor with knees bent and sitting with your legs stretched out with heels on another chair. The goal is to have your leg out straight while working on extension, and your knee flexed or bent to 90 degrees while working on flexion. The sooner you bend your knee and straighten it, the less pain you should have. Keeping your knee moving during the healing process is important for a full and speedy recovery.
If you are still in the hospital physical therapy will work with you again today, but most of our patients are home by now. If you are able to perform the exercises and you are medically stable, you may go home.
Dressing change and shower: You may remove your surgical dressing and shower two days after surgery. Roll the ace wrap back into itself as you unwrap your leg. The thick white cotton wrap may be pulled off your leg and discarded. If there is mesh glued to your incision, leave it until we see you at your follow-up. Shower, allowing water to run over the incision. Lightly pat your incision dry with rubbing alcohol and allow to air dry thoroughly before covering with sterile gauze and wrapping with the ace wrap. It may be easier to cut the ace wrap in half as you only need to wrap the knee and not the whole leg. Once you remove your bulky dressing, you can wear the white TED hose on both legs during waking hours. Remove the TED hose at night. If you have any question about your leg while changing the dressing, take a picture with your phone so you can show us.
Post-op Day 3: Practice all the physical therapy exercises you received from the hospital and our office until you are comfortable performing them. You will need to do these three times a day for 15-minute sessions each. Knee surgery patients who are planning to go to a rehab facility will be sent post-op day 3. Placement in inpatient rehab is done by your case manager and social worker and is dependent on insurance approval based on coverage and your progress. Familiar surroundings and the home environment generally provide a better recovery.
Post-operative Follow-up appointment:
To ensure your safe post-operative progression, your surgeon will ask you to return to the office 2 weeks after your surgery for x-rays and removal of staples, sutures, or tape from Dermabond glue. We will evaluate you at this time and give you the next level of exercises. We may recommend physical therapy start after your 2-week appointment, however, most of our patients have a full recovery with the simple exercises done at home. Your surgeon may ask to see you again at various intervals, for example, 6 weeks, 2 to 4 months, 6 months, and 1 year. For the long term, each patient is evaluated every two years with repeat x-rays and clinical exams. Any time you fall or have some kind of accident, it is a good idea to call us for an x-ray and appointment.
Information needed AFTER surgery
Keep ice on your knee as much as possible during the first few days. Twenty minutes every other hour or at least 3-4 times a day will help with pain and swelling. We highly recommend you rent a Game Ready by calling or texting the representative for Game Ready, Kameron, at 205-269-0200. Patients usually rent these machines for 2 weeks for $120 a week and return them to our office’s front desk at your 1st post op visit. Instead of using ice from your freezer or bag of ice in the ice machine, you can buy 14 8-oz bottles of water, freeze them, and use them instead. You will use 7 bottles in the machine at a time.
Use your walker or crutches as instructed until you feel safe and confident enough to go to a cane, crutch, or staff. The cane or staff should be used on the opposite side of the operative knee. When climbing stairs, remember the good leg goes up first to heaven and the bad leg goes down first to hell. Take 1 step at a time until you feel more comfortable.
If there are no contraindications, take an 81mg aspirin daily for 30 days after finishing your Xarelto, Eliquis, Plavix, Coumadin, Aspirin 325mg, or Lovenox to decrease the risk of blood clots. If you are on Coumadin, please have your medical doctor do the blood test required to check the levels 2-4 days after being discharged from the hospital to regulate the dose. This is very important.
Continue to wear your white TED hose support stockings (anti-embolism hose) on both legs for 4 weeks after surgery. You may remove them while sleeping. You may request a second pair before you leave the hospital, or you may purchase regular support hose elsewhere. For best results, lie down with your legs up for 30 minutes then put your hose on with your legs still up. If you put a plastic bag over your foot, the hose will slide on easier, then pull the bag out the toe hole when done.
You may shower on post op day 2. Remove the ACE wrap and bulky dressing on post op day 2 prior to showering. Allow water to run over the incision and pat dry with alcohol. Once your incision is dry, cover with sterile gauze and tape, pull the TED hose over your leg and wrap the ACE wrap from mid-calf to mid-thigh.
Either staples or glue (Dermabond) are used to close the skin after surgery. The staples or Dermabond tape are removed in the office 2 weeks after surgery. The tape from the glue is a very thin mesh which you can barely see. DO NOT REMOVE THE MESH TAPE. To make the removal of staples easy, apply polysporin to the incision for the two days before the staple removal appointment. If you have Dermabond tape do not use polysporin. You may use Mederma cream, Aloe Vera creams, Vitamin E Cream, or skin lotion on the incision after it has healed completely (approximately 3-4 weeks). Steri-strips will be applied after removing the staples and left on for 7 days. Remember no tub baths until after sutures or staples have been removed.
Reasons to Notify Us Immediately
- If you have a sudden increase in knee pain, which is not relieved by pain meds (Tylenol + NSAID + narcotic together), icing and elevating.
- If you have sudden increase in swelling, which does not decrease within 24 hours with elevation. Elevate your leg up on the wall, straight up, for 15 minutes 4x daily and also on a pillow under your leg at night.
- If you have large amounts of drainage from surgery site. Small amounts of blood, or clear yellow or blood-tinged serous fluid are normal. Creamy foul smelling yellow or green drainage is not normal. Please take a picture if there’s any question while changing your dressing to show us later.
- If you have increased pain, swelling, and redness in the calf or thigh, which doesn’t get better with pain medication and elevation. Do not massage a swollen red tight hot calf. If this happens after hours or on the weekend, go to the ER. This might be a blood clot.
- If you experience chest pain, shortness of breath, and/or coughing up bloody sputum, you will need to go to the ER immediately. This is a symptom of a possible blood clot.
We are here to help. If you believe you are in need of knee replacement surgery, we would love to deliver a diagnosis, get you treated and get you moving again.


