Replacing Your Worn-Out Hip
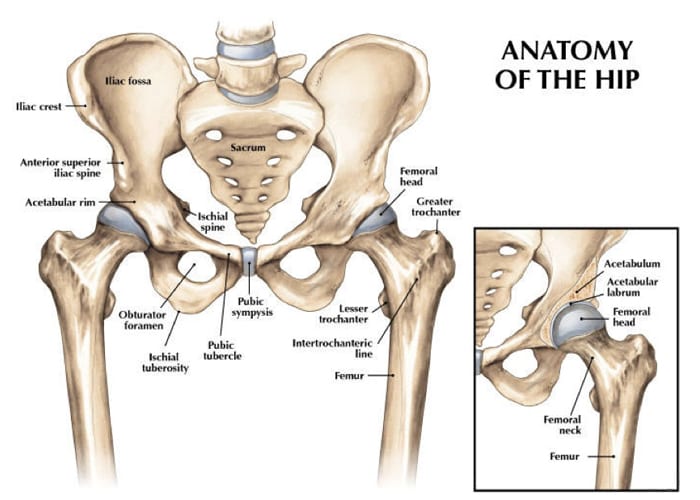
The goal of hip replacement surgery is to relieve pain and to improve function and stability. Hip surgery is commonly performed for reasons such as osteoarthritis, rheumatoid arthritis, avascular necrosis, trauma or problems from birth.
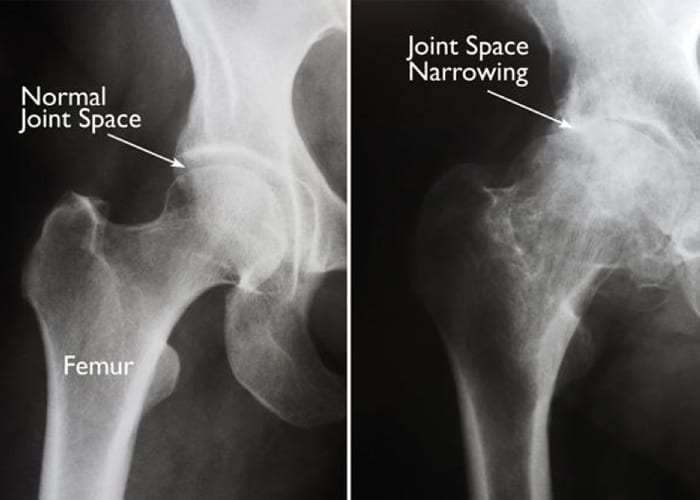
Degeneration of the hip joint can affect people of all ages. In the young, it often begins due to trauma in an automobile/motorcycle accident, football injury, falling off a horse or bicycle, or medication which causes the bone to lose its blood supply (avascular necrosis). It can be caused by gradual eroding diseases such as rheumatoid arthritis or lupus. The most common cause is simply normal wear and tear of the cartilage over a lifetime of use, and it is called osteoarthritis. In order to be considered for a total hip replacement there will be three major indications to have surgery. These are the severe pain you cannot stand it, inability to participate in activities you wish to do, and fear of falling.
Artificial hips typically last ten year to twenty years with an average life of 15 years. Since some bone is removed with each replacement, it is better to be in your 50’s or 60’s if possible before having your first hip replacement; however, we know that this is not always possible. To ensure the longest life possible for your artificial joint, it is best to maintain a normal weight and avoid high impact activities. You may still run or participate in sports once you are fully recovered, but this can increase wear on the prothesis requiring a revision surgery sooner. The best way to get the longest use out of a hip replacement is to maintain a healthy weight.
A regular x-ray of your hip will give us a realistic picture of what has happened to your bone. The x-ray, the history you give, and a physical examination of your hip will help your surgeon diagnose your condition. Even with all the sophisticated diagnostic tools available today, an x-ray is all that is needed majority of the time.
In the early stages of hip disease (degenerative joint disease), a program of exercise, such as a recumbent bike, swimming, weight control, and non-steroidal anti-inflammatory drugs (NSAIDs), can help decrease the need for surgical treatment. For people under the age of 50, conservative treatment is important to try to delay the need for the hip replacement until they are older. You will have lower risks of complications with prehabilitation and a speedier recovery. When conservative measures are no longer helpful and one meets certain criteria including weight and strength capacity, a total hip replacement is the next step to get your life back. We use minimally invasive, least invasive, surgical techniques to shorten your recovery process.
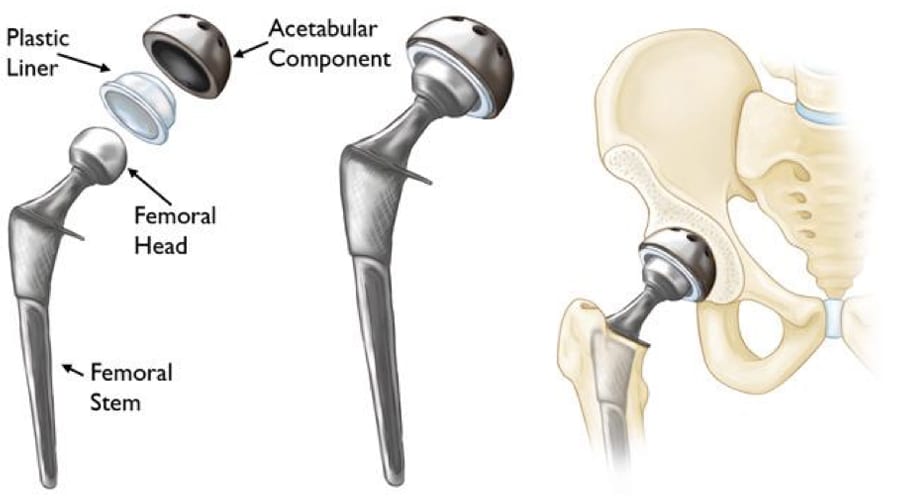
When a hip replacement is decided upon, a combination of metal and plastic are implanted to create a new joint that will glide painlessly with a greater range of motion than one has had in years. Many different prostheses exist, and specific details about you dictate the type selected. The metals used are extremely strong metals designed specifically for use in orthopedic surgery. Polymethyl-methacrylate (PMMA, commonly called “bone cement”) may also be used to hold the femoral component in place. Dr. Bramlett’s patients commonly receive a high-strength alloy hip through a minimally invasive technique avoiding internal muscle disruption. This gives you a faster recovery to your normal functioning after surgery.
For total hip replacement surgery, an incision is made down the lateral part of the hip, 4-6 six inches long. The femur and hip socket/acetabulum are exposed. The posterolateral approach is the best approach because it allows us to circumferentially debride diseased bone and tissue from around the joint, removing all sources of pain or instability, and allows good access to ream the femur for the best and most secure fit. The smallest amount of bone possible is removed and replaced with the metal and plastic components chosen for you. When the joint has been tested for maximum flexion, extension, rotation and stability of the hip (the hip does not dislocate easily), it is closed. A dressing is applied, and you are taken into the recovery room. The surgery itself takes approximately 30 minutes.
Complete recovery should be obtained within 2-6 months; yet, this is dependent on one’s health history. Physical and emotional preparedness prior to surgery are essential. The average is 3 months. Most patients progressively return to their normal day to day activities within 2-5 weeks, even though, healing will continue for weeks after that. Within a year you will forget you have an artificial hip. You may still have some stiffness with weather changes or increased activity, but your daily life will be much improved. Better quality of life is the main goal for this surgery. Eliminate pain and gain confidence in range of motion and function.
As with any type of surgical procedure, there are certain risks associated with hip surgery. These problems include dislocations, infection, swelling, blood clots, leg length discrepancy, nerve palsy, vascular injury, fractures, and pulmonary embolus. Rare complications do sometimes occur. Extensive measures are taken to prevent each of the above. You will be instructed in measures that will help to decrease the likelihood of problems and aid in a safe healing process. Your cooperation is vital in preventing many of the above complications.
You will be instructed to exercise to build up your stamina and strength and to diet or maintain a normal weight. This can be accomplished by swimming daily and/or riding a recumbent bicycle every other day for 30 minutes. Your cooperation is vital in your recovery process.
Total hip replacements are excellent procedures when chosen and performed correctly on appropriate patients. Your surgeon can provide you with information regarding the specific procedure and implant selected for you.
We hope that you find this information helpful. If any of the material in this booklet is unclear or if you have any questions, you may contact us at the office.
Thank you for taking the time to read this material. We understand that this manual contains a great deal of information. We also know that the best results come from the most informed patients and those motivated to see themselves in their best condition as quickly as possible.
Information needed Before surgery
- Total hip patients sometimes need to have a medical check-up before surgery with an internist or primary care physician. If you have any type of heart, kidney, or lung conditions, or you have had heart surgery, you will need to obtain a medical clearance letter from your physician. This is required in order to prevent any acute changes in your condition from occurring and will serve to ensure a safer, less complicated hospital stay.
- If your medications change from the time of your office visit until your surgery, please notify the office. It is always wise to keep a complete list of your medications and allergies with you, especially when coming to the hospital. If you have not gone to Pre-Admission Testing (PAT) you will need to bring all medicine bottles to the hospital on the day of your surgery.
- If you are taking aspirin or an arthritis medication such as Naprosyn, Aleve, Advil, Ibuprofen, Lodine, Voltaren, Feldene, Motrin, Relafen, or Daypro, you should stop taking it 5 days prior to your surgery date. You may continue Tylenol. If you are on a blood thinner such as Coumadin, Xarelto, Lovenox, Eliquis, Pletal, Pradaxa or any other prescribed medication which thins your blood you should check with your primary care physician or cardiologist to see how to transition off your blood thinner before surgery.
- If you smoke/vape or use any type of nicotine product, we want you to stop at least two weeks before surgery. Smoking increases the risk of respiratory problems and other complications that impede the healing process. Tobacco use is associated with higher infection risk. The cessation of smoking will enhance the overall improvement of your health and give your body the maximum opportunity to recover without complications.
- DO NOT EAT, DRINK, (NOT EVEN WATER OR ICE), SMOKE, CHEW GUM, OR EAT HARD CANDY after midnight the night before surgery. If you take any stomach, thyroid, or blood pressure medication in the mornings, you should take these with a sip of water the morning of your surgery. Pre-Admission Testing (PAT) will also go over which medications you should take the morning of your surgery.
- Work on the exercise program two times a day every day until surgery. Try to ride a recumbent-chair bicycle every other day for approximately 30 minutes. You will have a shorter recovery and lower complication rate if you do this.
- Arrange for family or friends to help you after being discharged from the hospital for the first week. A daily visitor or family member to assist with meals and a shower will make the transition easier. Please start preparing to return to a safe, familiar home environment. If you do not have any help, please let us know. Home Health Care or a rehab facility can be arranged at the hospital by a nurse case manager on the day of your surgery. Placement may be dependent on insurance clearance requirements.
- You will need to start showering with Hibiclens, Phisoderm, or Dial soap three days before your surgery. This will help guard against infection.
- The hospital or surgery center will call you the day before your surgery to discuss your arrival time for surgery. Please call us if you have not heard from us the afternoon prior to your surgery. Surgery times cannot be determined sooner due to surgery schedule changes and emergencies. Please disregard any e-mail you receive stating a time to arrive at the hospital for your surgery.
- Each hospital day is carefully planned, yet changes are not always predictable. Please be patient if your surgery or discharge is delayed.
- You will prepare to come to the hospital the day of your surgery. Upon arrival at the hospital you will check in at the admitting desk in the main lobby of the hospital.
- The average hospital stay for hip surgery is 1 night, with some going home the same day and some staying 2 nights.
- As with all medical information in this manual, please be sure to consult your surgeon’s office if questions exist. All details are beneficial to the overall clinical outcome.
What you SHOULD bring to the hospital:
- If you have your own crutches or walker, please bring them, and be sure to put your name on them. The hospital therapists will make needed adjustments. Otherwise the hospital will provide you with a walker or crutches.
- Bring loose fitting clothes. Your leg will be swollen following surgery. The day after surgery you will start dressing in these clothes instead of a hospital gown. We suggest a loose pair of shorts, a very loose pair of slacks or jogging pants, shirts, and comfortable walking shoes.
- Insurance cards unless you provided the hospital with this information at Pre-Admission Testing.
- Medications you are currently taking. Please bring the bottles if you did not go to Pre-Admission Testing.
- Bring a copy of the results of tests such as EKGs, Echocardiograms, stress tests, and clearance letters from your internists and/or specialist. This is in case we don’t receive these in our office via fax.
- Personal items, such as deodorant/toothbrush/razor.
- Living Will, if you have one.
What you SHOULD NOT bring to the hospital:
- Jewelry
- Unnecessary personal valuables
What you will need at home:
- Walker or crutches and a cane (a walker can be given to you at the hospital).
- Large zip-lock bags for ice or ice packs. You may make your own ice mixture by mixing 1 cup of rubbing alcohol and 3 cups of water into a zip lock bag and placing the bag in the freezer. It will be slushy and colder than a normal ice bag.
- Rubbing alcohol for cleaning the incision, along with tape and gauze pads for a dressing.
- Polysporin/Neosporin antibiotic ointment to apply to your incision 2 days before your follow up appointment IF you have staples.
- Someone to assist you with a shower and meals for a week once you return home.
- Tylenol and an NSAID or your arthritis medication for pain, headaches, or post-operative fever, which is a normal reaction of the body after surgery.
- A safe environment for walking, without loose rugs or cords, etc. Arrange your bedroom so
you can get in and out of bed easily.
- A firm bed that is easily accessible for rest. Chairs with high and firm seats with armrests.
- DO NOT sit in couches or recliners. Patients tend to sit in recliners or couches and reach for objects, which could put the operative leg in the wrong position causing it to dislocate your new hip.
Antibiotics Information
A joint replacement reacts much like a heart valve replacement to bacteria circulation within the blood stream.
It is required that you have an antibiotic before you have any dental/oral procedures for life.
You cannot have any dental work until 3 months after your surgery.
We can call in a prescription or your dentist can do this for you. The antibiotic protocol for implant prophylaxis follows: Amoxicillin 2.0 grams, taken orally one hour before procedure.
For amoxicillin/penicillin-allergic patients:
Clindamycin Adults, 600 mg given orally one hour before procedure
Cephalexin or cefadroxil: Adults, 2.0 grams orally one hour before procedure
Azithromycin or clarithromycin: Adults 500 mg orally one hour before procedure.
General Order of Events Following Surgery of the Hip:
Operative Day: After surgery you will arrive in your room with a dressing covering your incision. You may rest in bed, then stand at the bedside and/or sit in a chair. Make sure you have a nurse or physical therapist help you until you are safe getting up and down on your own. Once alert, we want you up and out of bed. You will be weight-bearing as tolerated with a walker; you will begin walking with the assistance of a physical therapist or nurse. Start doing your post-operative exercises, such as pumping your ankles to help with circulation. Also, press your knees down flat on the bed, locking your quads for extension. It is also time to do the frog abduction exercises. You can move any way that is comfortable for you. Initially you need to ask for help when turning to your side and getting out of bed. When turning from your back to your side be sure to use a pillow between your knees. You will be given a spirometer to use after surgery to help you breathe deeply; use it hourly while awake. You may start using a regular toilet the day of surgery. This will help to keep your lungs clear and prevent lung infections. Our patients get out of bed 3-6 hours post-operatively. After the first 6 hours bedpans and urinals should not be used. Plan on this as it starts the recovery process. If you are ambulating well and your pain is well controlled, you may go home the day of surgery.
Post-op Day 1: You need to eat all your meals sitting in a chair. Use the bed only for rest or sleep. If you are still in the hospital, the nursing staff and physical therapist will check to see if you are doing your exercises correctly. Initially, the physical therapist or nurse will help you get up and walk with you until you are independent. The nursing staff will also be assisting you in transfers from bed to chair if needed. These activities are important to your progress. Your drain will be removed, and a smaller dressing will be applied to your drain site prior to discharge. If a mesh dressing is on your incision leave this on until your post op visit. You may go home after you finish afternoon physical therapy and are medically stable.
Post-op Day 2: You will progress toward independently moving from bed to chair, exercising, and walking with a walker or crutches. You should be out of bed as much as possible. You should be getting up every hour during the day for 10 minutes. While sitting in the chair, practice lifting your knee and foot off the floor. While in bed, you should be working your legs into the frog position. This is a very safe position and will help you later for putting on your shoes. By consistently practicing this you should obtain a greater range of motion than you have had in years. You will also work on stair climbing. Most patients will be discharged before POD 2, with some requiring more monitoring or inpatient physical therapy at this point. If you are progressing slowly, transferring to a rehab facility may be the next step. The hospital social worker and case manager will arrange this with the facility and your insurance company.
If you are home, you may remove your surgical dressing and shower. Have somebody nearby to help if necessary. Allow hot water and soap to run over the incision and pat dry with alcohol. Leave the white mesh glued over the incision if present.
Post-op Day 3: Practice all the physical therapy exercises you received from the hospital and our office until you are comfortable performing them. Many hip surgery patients are able to return home on the 1st or 2nd post-op days. Most find home more comfortable once they are independent and medically stable. Hip surgery patients who are planning to go to a rehab facility will be sent post-op day 3.
Post-operative appointment: To ensure your safe post-operative progression, your surgeon will ask you to return to the office 2 weeks after your surgery for x-rays and removal of staples, sutures, or mesh from Dermabond glue. Your surgeon may ask to see you again at various intervals, for example, 6 weeks, 2 to 4 months, 6 months, and 1 year. For the long term, each patient is evaluated every two years with repeat x-rays and clinical exams.
Information needed AFTER surgery
Once home, with a total hip it is important to get up and move frequently. You need to get up every hour and walk around for 10 minutes during the day. Hip replacements do well, and people thrive on the lack of pain and sudden ability to be active again. Post-operative problems are uncommon, yet it is important to call your surgeon’s office if you have a sudden increase in hip pain, increased swelling which does not decrease with elevation, or pus draining from the incision (clear/yellowish or blood tinged drainage is normal). If you experience chest pain or shortness of breath, you should go to the emergency room immediately.
The following guidelines will apply for the next four weeks or until your surgeon allows changes:
- Use your walker or crutches as instructed until you feel safe and confident enough to go to a cane, crutch, or staff. This could take 1-2 weeks.
- If there are no contraindications, take an 81mg aspirin daily for 30 days after finishing your 2 week course of blood thinner (Xarelto, Eliquis, Plavix, Coumadin, Aspirin 325mg, or Lovenox) to decrease the risk of blood clots. If you are on Coumadin, please have your medical doctor do the blood test required to check the levels 2-4 days after discharging from the hospital to regulate the dose. This is very important.
- Use a pillow between your knees to turn in bed for approximately 2 months after surgery.
- Get in and out of bed on the side of the bed nearest to your surgical hip.
- Keep your knees 4 inches apart at all times when moving around for the first 2 months. In any situation, whether sleeping, sitting, getting in and out of the car, be careful to keep your knees apart for the first 2 months. This will enable you to relax and enjoy your hip for a long time.
- When sitting, choose an armchair for the first 2 months and anytime, thereafter if you have an option. It will make getting up and down easier, safer, and extend the overall life of your hip. For the first 2 months, do not sit on couches, low chairs, recliners or in bathtubs.
- An elevated toilet seat is unnecessary due to the method used to insert the hip; however, if your bathroom is a good distance from your bed, it might be helpful to have a bedside toilet to use at night. During the day, the arms of the toilet can be used over your regular toilet to assist you.
- Continue to wear your support stockings (anti-embolism hose) for 4 weeks after surgery. You may remove them at night for comfort. You may request a second pair before you leave the hospital, or you may purchase regular support hose elsewhere.
- Surgical stainless-steel staples or Dermabond, a type of glue, are used to close the skin after surgery. The staples or Dermabond tape are removed in the office 12-16 days after surgery. The tape from the glue is a very thin mesh which you can barely see. DO NOT REMOVE THE MESH TAPE. To make the removal of staples easy, apply Polysporin/neosporin to the incision for the two days before the staple removal appointment. If you have Dermabond tape do not use polysporin. You may use Mederma cream, Aloe Vera creams, Vitamin E Cream, or skin lotion on the incision after it has healed completely (approximately 3 weeks). Steri-strips will be applied after removing the staples and left on for 7-10 days. Remember no tub baths until after steri-strips have been removed.
- Ice your hip every hour for 20 minutes after surgery. This will help with the pain and swelling.
Medications
Your prescription after surgery will consist of pain medication, usually either Norco or Percocet. Phenergan or Zofran may also be given for nausea if needed. You will also receive Robaxin for muscle spasms. You may resume your anti-inflammatory medicine (Advil, Mobic, Celebrex, Lodine, Indocin, or Aleve) the day after surgery. Pain medication and anesthesia can cause constipation, so increase the bulk in your diet; and if needed, you can take a laxative. Over-the-counter medications are less likely to cause this problem so the sooner you can get off pain medicine the better you will feel.
Tylenol and Advil or Aleve can be taken together for pain to help decrease the need for narcotics. Two and Two, Twice a day will help reduce pain and narcotic use. (2 Tylenol & 2 Advil/Aleve together twice daily). If you have a prescription arthritis medication that takes the place of Advil/Aleve.
You will be given a blood thinner after surgery to prevent blood clots. This will usually be either Eliquis of Aspirin which you will take twice daily. After completing this two-week course, you will either resume your home blood thinner or you will take a baby aspirin (81 mg) daily for 1 month. If you are on Eliquis, you should not take anti-inflammatory medicines until you finish with the Eliquis (this includes Advil, Aleve, Celebrex, Naprosyn, Mobic, Lodine, etc.)
You may resume the remainder of your home medicines the next morning after surgery.
Sleep
If you have difficulty sleeping, we recommend a hot shower right before bed. You can also take your muscle relaxer (Robaxin/Methocarbamol) and/or Benadryl to help you sleep.
Picking Up Objects from the Floor
Begin by practicing standing on the operative leg, squat (bend) slightly on the one leg and hold for a minute. As you get stronger, go lower with the squatting position. Alternate working with both legs. You may start this as early as you want, usually around two weeks. When you feel strong enough to get to the ground safely, begin by holding on to a table, chair, or wall for balance. Kneel down on the knee of your non-operative leg. Once you are stable, bring your other knee down so that you are in a kneeling position. Finally, spread your knees apart. You are in the correct position. To get back up, reverse the process you just followed. Hold onto something for support. It is important to always have someone with you the first few times you practice this technique. You should gain strength before trying this alone. Hold onto a piece of heavy furniture, such as an armchair, with the opposite hand. Stand on the non-operative leg and lift the affected leg (straight) behind you while bending down to pick up the object. You must have good strength in order to do this safely.
Putting on Socks and Shoes
Sit in a chair and put your foot on a stool with knee rolling outward. It is safe to reach and do these activities in this manner. Never put your shoes on by bending at the waist and putting your foot out to the side allowing your knee to bend and roll inward. This can cause dislocation of the hip. Women shaving their legs or applying lotion sometimes use this same improper movement. More problems are experienced following hip surgery by people attempting to do these things than any other activity.
Getting Into and Out of a Car
Getting in the car should be done keeping your knees apart at all times. Back into the seat, holding onto the car door and the seat back. Sit down and bring one leg in and then the other. Remember to keep your knees separated, heels turned inward and foot pointed out, and knee outward as if you are keeping a ball between your knees. Have the seat pushed as far back as possible and the back of the seat tilted, so you will have more room.
TOTAL HIP EXERCISES
Physical Therapy
During your hospitalization, physical therapy is a vital part of your recovery. Do the frog exercises, the leg squatting exercises by holding on to your walker or a counter, and the alternating leg lunges. These are described below. It helps you to regain your full potential. Once at home, continue to do the exercises you were given in the hospital four times a day. Start using your stationary bicycle with the seat at a comfortable height about 3-4 weeks after surgery. Remember to ride your bicycle every other day, not every day. In addition to your exercises begin walking on flat, even ground. Start with walking 10 minutes per day, and each week add another 5 minutes so you will be walking 30 minutes-1 hour, three to four days per week. Outpatient physical therapy will be addressed at the time of your first post-operative office visit. Always ice your hip after exercising.
The following are some exercises you must do, particularly as you make preparations for your hip surgery. Work out 20-30 minutes, twice a day before surgery and three to four times a day after surgery. Remember to start out slowly and that with any new exercise program you will probably have increased muscle soreness and pain. Please, continue and work through this phase.
After about 3 weeks you will find everything becoming easier. Each exercise protocol has been tested and developed during 20 years of successful implementation and follow up. They are designed to help you and will not impair or harm.
Exercises Before Surgery-Phase 1
Ankle Pumps
Ankle pumps help prevent the development of blood clots. Lie on your back or sit in a chair. Pull your toes toward you and hold for 5 counts. Point your feet and toes downward and hold for 5 counts. Relax for 10 counts. Be sure to generate full force in both directions. Before your operation, do 30 ankle pumps in the morning and 30 in the afternoon, plus anytime in between. You will resume this exercise when you awaken in the recovery room.
Quad Sets
Quad sets help you gain leg control after surgery and improve circulation. Lie on a bed. Point the toes of your foot on your operative leg toward your face. Now tighten your thigh muscle and press the back of your knee down touching the bed. Hold for 10 counts and relax. You need to do this exercise 30 times, twice a day. You will also do this exercise immediately after surgery. This exercise can be combined with some of your other exercises, such as your gluteal sets. Both are critical to your ability to transfer in and out of chairs.
Knee Extensions
Knee extensions also will assist you in moving from the bed to the chair and from the chair to a standing position. Lie on the bed. Place a roll of towels (the size of a 3-liter soda bottle) under your knee. Push the back of your knee down on the roll and tightening your quadriceps muscle on the top of your leg. This will cause your lower leg to straighten and your heel to come off the bed. Pull toes toward your face to tighten the entire leg. Hold for 5 counts and relax, allowing your heel to go back down to the bed. Rest for 5 seconds and repeat. You need to do this exercise 30 times, twice a day.
Lunges
Holding onto your walker or counter, standing up straight, take your right leg and lunge forward approximately 3 feet making sure to keep back upright and straight. Hold for 10 seconds. Go back to standing up straight. Lunge forward with the left leg. Hold for 10 seconds. Do these 5 times, three times a day.
Knee Bends Standing up
With legs apart approximately 2 to 2 1/2 feet between feet and holding onto walker or counter, bend at the knees 1/3 of the way to the floor, hold for 10 seconds. Do these 5 times, three times a day.
Stationary or Recumbent-Chair Bike
Before surgery, you should use a recumbent-chair bicycle to build up your endurance to ride it at least 30 minutes every other day. Normal to light resistance is all that is required. Begin riding the bicycle 2-3 weeks after surgery. Start with 10 minutes and work up to 30 minutes every other day. Icing your incision 10 minutes before and after each exercise for the first 2 weeks may make you more comfortable. If you do not have a recumbent bike, it is very likely that a relative, friend, church, or exercise club may have one that you can use. This is an exercise which should be done 3 times a week for the rest of your life. It is something that is safe and will benefit your general health and improve your quality of life.
Swimming
Swimming is also an excellent exercise. If possible, swim 20-30 minutes, at least three times a week. You may resume swimming 2-3 weeks after surgery. We prefer using a float (noodle) to assist floating and tread water for 4-6-minute intervals 4-6 times each pool session.
Chair Exercise 90 degrees – 90 degrees
This exercise begins after surgery and helps you regain control of your muscles, enabling you to lift your foot to take a step or get into the car. It is simple, but effective. To do it, sit in a chair with your hips and knees at 90-degree angles. Both feet should be flat on the floor. Without using your hands, lift the foot of the affected leg up so that the sole of your foot clears the floor. Hold this position for as long as you can. Continue to improve on your time until you can hold your foot off the floor for 2-3 minutes.
Exercises After Surgery-Phase 2
The way you perform various functions after surgery, like putting on socks and shoes, becomes very important. This is because picking objects from the floor and getting in and out of cars involves moving your hip. The most frequently seen complication after hip surgery is dislocation of the hip joint. You need to remember that the new hip does have limitations and you need to learn to avoid positions which might lead to dislocation. Here are three exercises you need to start after your surgery and continue as you return home. These assure proper hip position and movement. They also allow you to function safely in your home.
Most of our patients can expect a full recovery with our home exercise program. We will evaluate you at your 2-week follow-up appointment and may recommend seeing an outpatient physical therapist at that time, however, you will need to do you exercises at home 3-4 times a day for a full recovery.
Frog Abduction
Frog abduction is important to ensure full range of motion after surgery and will result in decreased pain and minimization of scar tissue. You may start this the day of surgery. Lie on your back. Slide your feet toward your body so that your knees are in the air and feet are flat on the bed. Now spread your knees out to the sides. You may have to push them and it is OK to have someone help by applying gentle but firm pressure. You will not cause damage to your hip by doing this. Hold for 2 minutes and then repeat. Once you can frog lying down you can start holding rigid support, such as a walker, furniture, etc. and standing up and squatting in slow manner to hold your position. This really builds strength and eliminates your limp.
Lunges
Holding onto your walker or counter, standing up straight, take your right leg and lunge forward approximately 3 feet making sure to keep back upright and straight. Hold for 10 seconds. Go back to standing up straight. Lunge forward with the left leg. Hold for 10 seconds. Do these 5 times, three times a day.
Knee Bends Standing up
With legs apart approximately 2 to 2- 1/2 feet between feet and holding onto walker or counter, bend at the knees 1/3 of the way to the floor, hold for 10 seconds. Do these 5 times, three times a day.
Walking
When you are discharged home, be sure to get up every hour during the day and walk around for 5 – 15 minutes.
Climbing Stairs
Yes, at first you will climb the stairs the same way you did before surgery: by climbing one stair at a time going up the stairs with the non-surgical leg, and going down the stairs using the surgical (bad) leg. Very soon you will climb them in a normal way. You will be instructed to safely do this before your discharge.
Things to Avoid Doing That Can Cause Your Hip to be Dislocated
- Putting on socks, shoes and hose improperly by rolling the knee inward
- Picking up things from the floor improperly by rolling the knee inward
- Sitting on seats which are too low and rolling the knee inward
- Turning your body before your hips and leg
- Not having a pillow between your legs when lying on your side
- Putting lotion on or shaving your legs improperly by rolling leg inward to an extreme
- Consuming alcohol to the point of relaxing the muscles around the hip or causing a fall
Dislocations are events that occur less than one percent of all cases. Ninety percent of dislocations are caused by rolling the leg inwardly to the extreme. It is easy to avoid and easily prevented.
Frequently Asked Questions
What should I watch for concerning blood clots?
The chances of a blood clot occurring are low. All the exercises you are performing assist in eliminating this occurrence. If you experience the following symptoms, please notify either your surgeon or primary care physician. If you think you may have a blood clot, do not massage the area.
- Leg swelling that does not change after sleeping and elevation
- Skin that is shiny and tight from swelling
- Severe pain and heat in the calf or groin.
- If the leg is swollen, shiny, the swelling does not go down any through the night with elevation, the swelling is accompanied by sudden pain in the calf or groin especially when doing the ankle pumps, please call your surgeon during the day or go to the ER after hours.
- Shortness of breath or pain in chest when breathing.
I’ve noticed some drainage from my incision. Is this normal?
Yes, it is not uncommon to see a clear yellow or blood-tinged drainage up to 2 weeks after surgery. Drainage does not always indicate an infection. Continue to shower and clean the incision with alcohol daily. Leave the incision covered with a dry dressing until your 2-week post-op appointment. Apply Polysporin/Neosporin ointment to your incision 2 days before your office visit for easier staple removal.
What signs of infection would be of concern?
- A change in pain to a more constant, severe pain, whether standing, sitting or lying down.
- Very red and angry (warmth and mild to moderate redness is normal).
- A thick drainage, color creamy yellow to green.
- A temperature of over 101.5 degrees for 36 hours. (A temp of 99-101 degrees, off and on, for two to three days after surgery is a normal response).
What is a good policy regarding sitting or lying around?
Initially, it is best not to sit longer than fifty minutes at a time. You must get up and walk around every hour for 10 minutes. Constant up and down activity is helpful. This will help decrease the risk of blood clots and stiffness.
When can I begin driving a car?
We routinely allow our patients to drive a car when they feel it is safe, usually after your first post-op visit and you didn’t have surgery on your right hip. Do not drive until you have complete control of your right leg and are no longer taking pain medication. One test to begin driving again is to sit in a chair and if you can pat the operative foot and lift the entire leg with control then you may start driving again as long as you are not taking pain medication
May I cross my legs?
Yes, ankle on the knee (this is referred to as the “figure 4”) is fine or ankle on ankle. DO NOT cross your legs at the knees, as is common with women, until you have gained leg and function control.
May I turn to my side or stomach while lying down?
Yes, you may turn to either side but you should do so with a pillow between your knees to keep them apart. This is a necessary precaution to prevent a hip dislocation, especially for the first two to three months. To turn on your stomach you can straighten the legs firmly and roll over.
Please call office if any problems arise or if you have any questions.
We are here to help. If you believe you are suffering from one of these conditions, we would love to deliver a diagnosis, get you treated and get you moving again.


