What is Advanced DJD?
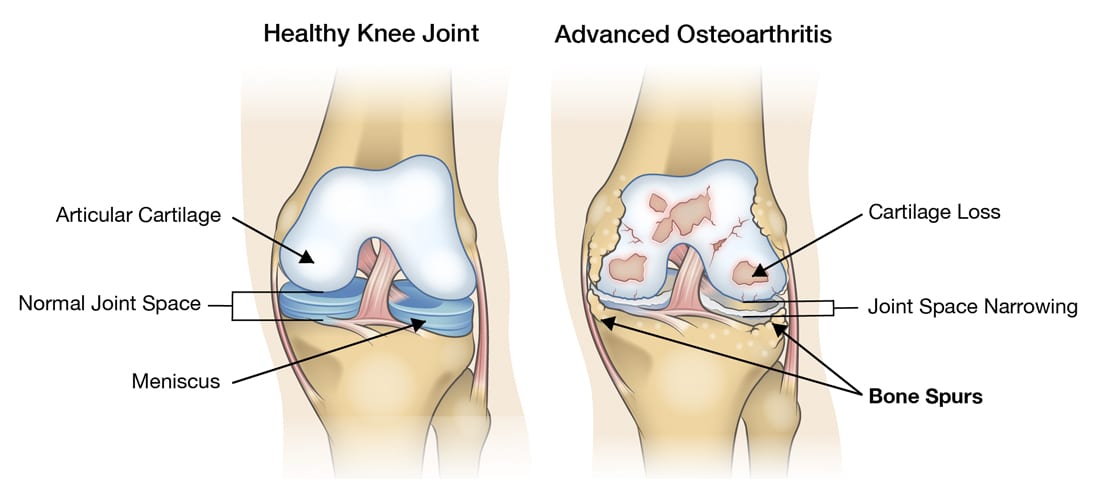
Advanced DJD (Degenerative Joint Disease) of the knee is the breakdown of the cartilage and instability of the knee which causes pain, swelling, loss of motion and activity. In knee osteoarthritis the cartilage protecting the bones of the knee slowly wears away. Your knee is divided into three major compartments: the medial compartment, the inside of the knee; the lateral compartment, the outside of the knee; and the patellofemoral compartment, the front of the knee between the knee cap and thighbone.
Advanced osteoarthritis in the knee can be limited to a one, two or all three compartments (tri-compartmental osteoarthritis). Unicondylar knee arthroplasty can replace the medial compartment, leaving the remaining joint surfaces intact. A patellofemoral joint (PFJ) arthroplasty can replace the surfaces on the back of the kneecap. These are more conservative that a total joint replacement and allow for a quicker recovery. In cases of two or three compartment DJD, a total knee arthroplasty is indicated. This is one of the most common orthopedic procedures performed in the world.
How does Advanced DJD occur?
Advanced degenerative joint disease (DJD) of the knee’s compartments is commonly from everyday wear-and-tear activities. It can be hereditary, but most often it is the degenerative type that comes with overuse and the aging process. Injuries, mal-alignment, and obesity will all accelerate the development of knee pain and DJD.
What are the symptoms of Advanced DJD?
A knee joint affected with advanced osteoarthritis will be painful and inflamed. Uni-compartmental arthritis will have localized pain to one area of the knee (usually the medial compartment). Tri-compartmental osteoarthritis will have radiating pain and stiffness across the entire knee joint. While pain, stiffness, and trouble bending the knee are characteristic of osteoarthritis, grinding, catching, swelling and locking symptoms may also be present. Weakness and buckling at the knee will occur with advanced osteoarthritis causing falling due to instability; this requires immediate attention.
How is Advanced DJD diagnosed?
A complete history and physical examination will be performed. There is typically swelling, redness, tenderness, decreased range of motion (ROM), crepitus (popping/crackling at the joint), and pain with weight bearing and instability of the joint. Routine x-rays of the joint will be done that will usually show joint space narrowing, sclerotic changes in the bone, and bone spurs in the arthritic compartments. DJD of the knee is easily diagnosed in most cases.
How is Advanced DJD treated?
Nonsurgical treatment of advanced DJD starts with lifestyle changes. Minimizing activities that aggravate the condition such as switching from high impact exercise to lower impact exercises such as riding a bike or swimming is very helpful in early and late stages of osteoarthritis. Losing weight is a very important factor in avoiding surgery and in reducing your pain levels.
We can give you home exercises to do or prescribe outpatient physical therapy to help increase strength and mobility while reducing pain. Special braces may be recommended based on your needs. Different modalities to reduce pain and inflammation such as ice and heat application, pain relieving ointments like over the counter Voltaren Gel, and oral medications including over the counter pain relievers, non-steroidal medications, and the COX-2 inhibitors Celebrex (celecoxib) or Mobic (meloxicam) can be tried. There are numerous injections that we provide for pain and inflammation relief such as corticosteroid injections (Zilretta) or viscosupplementation (Gel-One).
As the pain advances and the joint spaces are minimal, surgical intervention is your option to get back to doing the things you love. Advanced DJD in one compartment requires a unicondylar knee arthroplasty (half knee replacement). The only compartment that is replaced with metal and/or plastic is the articulating surfaces between the compartment that is arthritic such as the medial or patellofemoral compartments (as shown on right). This preserves the bone and cartilage in other healthy compartments of the knee.
Advanced DJD of all three compartments requires a full or total knee arthroplasty (TKA). Metal and plastic materials are used to completely replace the articulating surfaces (as shown on left). The damaged cartilage and bone at the distal end of the femur and proximal end of the tibia are carefully removed, and you leave the operating room with a well-operating knee joint. With a minimally invasive knee replacement, only 4-8 mm of bone is removed (approximately ¼”) in order to implant the prosthesis.
What is the recovery time for Advanced DJD treatment?
Your partial or total knee replacement can be done in the hospital as an inpatient procedure or outpatient surgical center, and you can go home the same day in most cases. Surgical techniques and anesthesia improvements as well as good education allows patients to be better prepared and clearer of their post-operative requirements.
A few hours after surgery you will be up and walking and start range of motion (ROM) exercises. Some patients may need to use crutches or a walker depending on their conditioning and strength before surgery for a few days to gain mobility in the knee operated on. You may bear full weight as tolerated on your operative knee immediately after surgery. We have designed a home exercise program to return you to maximal functioning. You will do these exercises on your own at home three times a day until we see you for your 2-week follow-up appointment. At this time, we will advance you to the next set of exercises. Outpatient physical therapy may be recommended at your follow-up appointment, however, most of our patients are able to have a full recovery with our home exercise program. You may resume light sports activities in 6 weeks, with no restrictions after 6 months.
We are here to help. If you believe you are suffering from one of these conditions, we would love to deliver a diagnosis, get you treated and get you moving again.


